RSV Diagnostic Testing Trends Reflect Evolving Protocols
Published: 2025-07-24
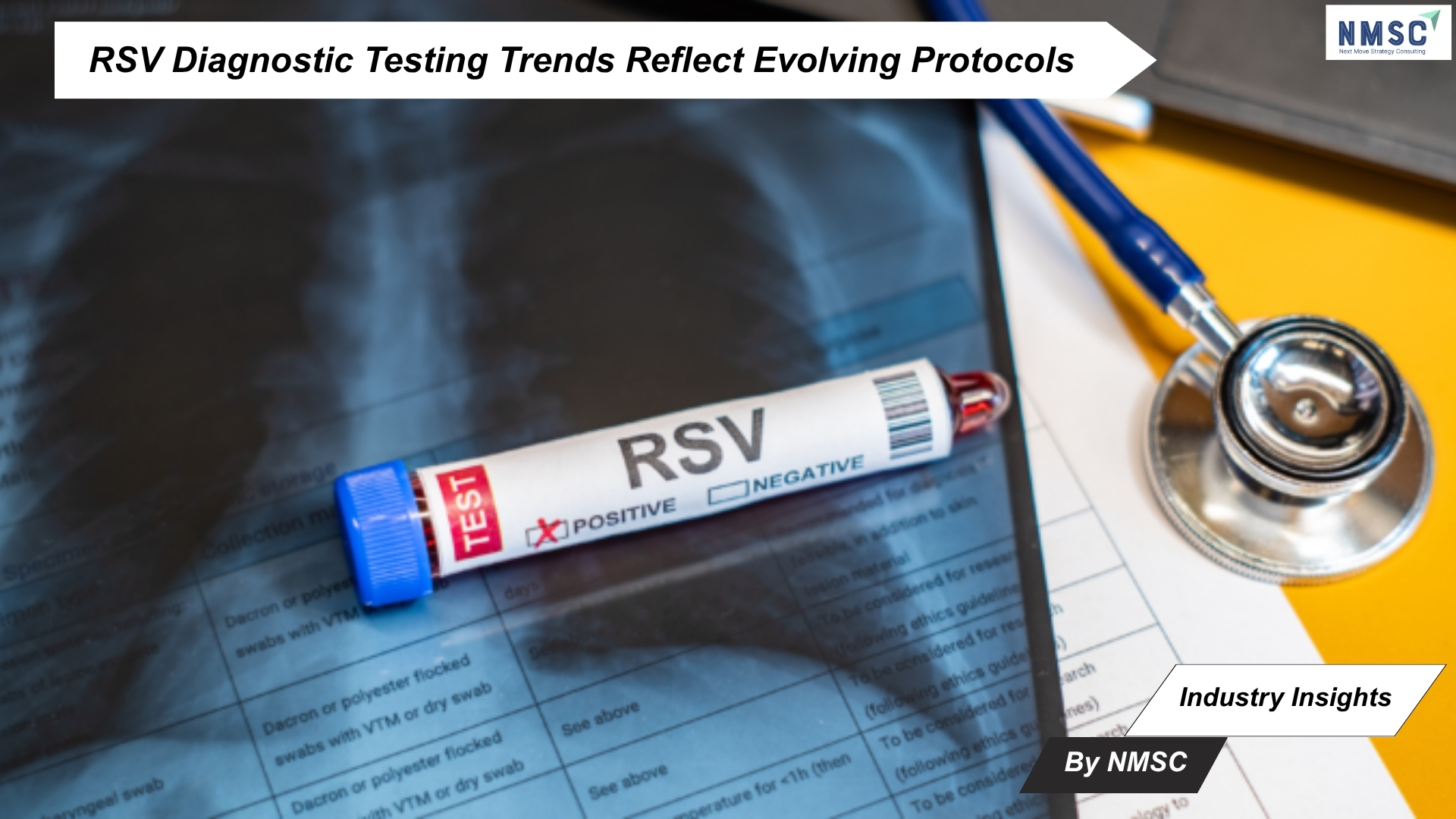
Industry Insights from Next Move Strategy Consulting
Amid ongoing efforts to improve respiratory illness management, new research underscores a significant link between Respiratory Syncytial Virus (RSV) detection trends and the diagnostic protocols used. Researchers writing in Swiss Medical Weekly noted that although respiratory syncytial virus (RSV) has traditionally been viewed as a childhood illness, it is now increasingly acknowledged as a significant cause of respiratory disease in adults—especially among those who are immunocompromised or over the age of 65.
Study Analyzes RSV Cases and Detection Trends Amid Shifting Public Health Measures
Neal Breakey, MD, and his team conducted a study at a single hospital spanning from 2016 to 2023, investigating the clinical and epidemiological profiles of patients who tested positive for RSV using reverse transcription–polymerase chain reaction (RT-PCR). Their analysis covered predisposing factors, patient demographics, treatment strategies, and clinical outcomes. The researchers also examined how RSV detection patterns shifted in response to evolving testing protocols and public health interventions, particularly during the COVID-19 pandemic.
Key Findings from RSV RT-PCR Testing and Patient Analysis (2016–2023)
-
A total of 8,135 RT-PCR tests were conducted between 2016 and 2023.
-
231 tests (2.8%) returned positive results for RSV.
-
The average age of RSV-positive patients was 69 years.
-
Complete clinical data were available for 194 patients.
-
81.0% (n=157) of these patients required hospitalization.
-
12.0% (n=19) of the RSV cases were identified as nosocomial infections.
-
Most common symptoms among RSV-positive patients:
-
Sore throat: 73.0
-
Dyspnea: 44.
-
Fever: 39.0%
-
-
Comorbidities observed:
-
Cardiac disease: 54.0%
-
Pulmonary disease: 49.0%
-
Anemia: 43.0%
-
-
Only 21.0% of RSV-positive patients were treated in an outpatient setting.
Evolving Testing Strategies Reveal Shifts in RSV Detection and Seasonal Trends
The significant rise in RSV testing and diagnoses following the lifting of pandemic restrictions was consistent with findings from other studies in the United States and Europe. According to Dr. Breakey and his team, this trend may be attributed to several extended and early winter seasons in their region, which likely contributed to higher RSV prevalence. They also suggested additional contributing factors, such as heightened hygiene practices, decreased early childhood and prenatal exposure to RSV during the pandemic, and modifications in testing protocols.
The researchers noted that the move from targeted RSV testing to broader respiratory virus panels reflects the progression of diagnostic technologies. They pointed to their own shift from trivalent to quadrivalent PCR testing—prompted by testing changes during the pandemic—as a clear example of this transition.
They also emphasized that the changes in RSV detection observed during the study mirrored shifts in testing practices, underscoring the complex relationship between diagnostic approaches and recorded disease trends within a regional hospital context.
Conclusion: Advancing RSV Diagnostics to Strengthen Public Health Response
The study led by Dr. Breakey highlights how evolving diagnostic protocols, especially during and after the COVID-19 pandemic, have directly influenced the detection and understanding of RSV. With increasing recognition of RSV’s impact beyond pediatric populations—particularly among older and immunocompromised adults—the need for consistent, comprehensive testing strategies is more pressing than ever. As diagnostic technologies continue to advance and broader testing becomes the norm, aligning clinical and surveillance approaches will be critical to improving disease monitoring, guiding treatment decisions, and informing effective public health responses.
Source: https://smw.ch/index.php
Prepared by: Next Move Strategy Consulting














Add Comment