Health Insurance TPA Market by Insurance Type (Group Health Insurance, Individual Health Insurance, Others), by Service Type (Claims Processing, Pre-Authorization), by Deployment Model (In-House TPAs, Outsourced TPAs), by Sales Channel (Direct Selling, Agents, Brokers), by Enterprise Size (Small & Medium Enterprises, Large Enterprises), and by End Users (Insurance Companies, Hospitals & Healthcare Providers, Others) – Global Opportunity Analysis and Industry Forecast, 2025–2030
Industry Outlook
The global Health Insurance TPA Market size was valued at USD 223.03 billion in 2024 and is predicted to reach USD 235.29 billion by the end of 2025. The industry is predicted to reach USD 307.52 billion by 2030 with a CAGR of 5.50% from 2025 to 2030. The industry is witnessing robust growth driven by rising health insurance penetration, expansion of hospital networks, and increasing adoption of digital technologies.
Growing awareness of financial protection, government initiatives, and wider insurance coverage are fuelling demand for efficient claims management, cashless settlements, and customer support services. The integration of hospitals into insurer-approved networks further enhances the role of TPAs in coordinating seamless healthcare access.
At the same time, digital transformation through AI, automation, and blockchain is boosting operational efficiency and customer satisfaction. However, stringent and varying regulatory frameworks across regions pose compliance challenges. Looking ahead, the integration of wellness and preventive healthcare programs offers significant opportunities for TPAs to expand their service scope and strengthen the market presence.
Rising Health Insurance Penetration Drives the Market Growth
The increasing adoption of health insurance policies worldwide is a major driver for the health insurance TPA market growth. Growing awareness of financial protection against medical expenses, coupled with government initiatives to expand health insurance coverage, has significantly boosted policyholder numbers across both group and individual segments.
As more people come under the ambit of health insurance, the volume of claims and administrative transactions rises sharply, creating strong demand for TPAs to manage claims processing, cashless settlement, and customer support efficiently. This expanding insured population directly fuels the need for professional TPA services, making rising medical insurance penetration a critical growth catalyst for the sector.
Expansion of Hospital Networks Fuels Market Expansion
The rapid growth and integration of hospitals into insurer-approved networks are significantly driving the health insurance TPA market expansion. As insurers and corporates seek to provide wider access to healthcare facilities for policyholders, TPAs play a vital role in managing and coordinating these extensive hospital partnerships.
Larger hospital networks require efficient administration of cashless claims, standardized billing, quality monitoring, and timely settlement processes, all of which fall within the scope of TPA services. This expansion not only enhances convenience for patients but also increases reliance on TPAs to ensure seamless connectivity between insurers, hospitals, and policyholders, thereby fuelling the health insurance TPA industry growth.
Digital Transformation & Automation Boosts the Market Demand
The adoption of digital technologies such as AI, machine learning, blockchain, and robotic process automation is transforming the way TPAs operate. These technologies enable faster claims adjudication, fraud detection, seamless customer support, and real-time tracking of policyholder services. Digital platforms also allow TPAs to integrate with insurers and hospital networks more efficiently, reducing manual errors and turnaround times.
As policyholders increasingly demand transparency, speed, and convenience, TPAs leveraging digital transformation are better positioned to deliver value-added services. This shift toward automation and digitalization is a key growth driver, improving operational efficiency and enhancing customer experience across the health insurance ecosystem.
Regulatory and Compliance Challenges Limits the Market Growth
The health insurance TPA market expansion faces significant challenges due to stringent regulatory frameworks that vary across countries. TPAs must comply with complex guidelines related to data privacy, claim transparency, service quality, and standardization set by insurance regulators and health authorities.
Frequent changes in rules, coupled with high compliance costs, slows down operational efficiency and limit scalability, especially for smaller TPAs. Inconsistent regulations across regions also create barriers for global players looking to expand. These regulatory and compliance hurdles act as a restraint, increasing operational risk and reducing flexibility in service delivery.
Integration of Wellness and Preventive Healthcare Programs Creates New Growth Opportunities
Beyond traditional claims management, TPAs have a growing opportunity to expand into wellness and preventive healthcare services. With rising focus on reducing long-term healthcare costs, insurers and corporates are increasingly promoting preventive care, employee wellness, telemedicine, and digital health monitoring.
TPAs leverage their existing role as intermediaries to integrate these services, offering health check-up packages, lifestyle management programs, and digital wellness platforms. This not only strengthens their value proposition to insurers and corporates but also creates new revenue streams while improving customer retention. As healthcare shifts from treatment to prevention, TPAs are well positioned to capitalize on this emerging opportunity.
Market Segmentations and Scope of the Study
The health insurance TPA market report is segmented by insurance type, service type, deployment model, sales channel, enterprise size, end users, and regions. Insurance types cover group health, individual, and others, serving diverse policyholder needs. Service types include claims processing, pre-authorization, cashless settlement, customer support, and hospital network management, ensuring efficient healthcare access. Deployment models are categorized into in-house and outsourced TPAs, while sales channels span direct selling, agents, and brokers. By enterprise size, the market is divided into SMEs and large enterprises. End users include insurance companies, hospitals & healthcare providers, corporate sector, and others. Regionally, the market is analysed across North America, Europe, Asia-Pacific, and the Rest of the World.
Geographical Analysis
In North America, escalating healthcare expenses are a major factor driving the health insurance TPA market share. According to the American Medical Association (AMA), U.S. health spending rose by 7.5% in 2023, reaching USD 4.9 trillion in 2025, highlighting the financial burden on insurers, employers, and individuals. This surge in costs has intensified the need for TPAs, which help manage claims efficiently, negotiate with hospital networks, and ensure transparency in billing. By enabling cost containment while improving service delivery, TPAs are becoming increasingly vital to the region’s health insurance ecosystem.
The rising elderly population is a key driver of the sector in Europe. According to Euro News in 2025, the share of individuals aged 80 and above in the EU is projected to increase 2.5 times between 2024 and 2100, from 6.1% to 15.3%. This demographic shift will significantly increase demand for healthcare services, including hospitalization, chronic disease management, and long-term care.
As the volume and complexity of claims grow, TPAs play a vital role in ensuring efficient claims processing, cashless treatment access, and smooth coordination between insurers and healthcare providers. The aging trend strengthens the reliance on TPAs to sustain Europe’s healthcare and insurance systems.
The growing burden of chronic illnesses is a significant driver of the health insurance TPA market in Asia-Pacific. According to the Institute of Public Health Bengaluru in 2025, India alone has over 266 million tobacco users, with tobacco-related diseases causing 1.2 million deaths annually and imposing an economic cost of around USD 12.5 billion per year.
Tobacco consumption is a major risk factor for chronic conditions such as cancers, cardiovascular diseases, respiratory illnesses, and diabetes. As these health challenges intensify, the need for frequent treatments and long-term care leads to a surge in insurance claims. TPAs play a critical role in managing this rising demand by ensuring efficient claims processing, cashless healthcare access, and effective coordination between insurers and providers across the region.
In the Rest of the World (RoW), particularly across Latin America, the Middle East, and Africa, expanding health insurance penetration is a key growth driver for the TPA market. Governments and private insurers are increasingly introducing affordable health insurance schemes to improve access to healthcare, especially in underserved populations. This expansion is generating a sharp rise in the number of policyholders and, consequently, in claims volumes.
TPAs are instrumental in managing these claims, ensuring transparent billing, and building hospital networks that support cashless treatment. As health insurance coverage broadens across emerging economies, TPAs are becoming essential partners in strengthening healthcare systems and improving service delivery.
Strategic Innovations Adopted by Key Players
Key players in the health insurance TPA industry are actively pursuing digital solutions, policy updates, and member engagement initiatives to strengthen their market presence and meet evolving healthcare and insurance demands.
-
In July 2025, UMR published an Administrative Guide for providers offering commercial and Medicare Advantage services.
-
In June 2025, UMR released its July 2025 Medical Policy Update Bulletin, featuring revised medical and drug policy guidelines effective from July–September 2025.
-
In April 2024, Meritain announced the launch of OnPoint Solutions, a member-centric program aimed at reducing cost of care through enhanced engagement and support tools.
Key Benefits
-
The report provides quantitative analysis and estimations of the industry from 2025 to 2030, which assists in identifying the prevailing health insurance TPA market opportunities.
-
The study comprises a deep-dive analysis of the current and future health insurance TPA market trends to depict prevalent investment pockets in the sector.
-
Information related to key drivers, restraints, and opportunities and their impact on the market is provided in the report.
-
Competitive analysis of the key players, along with their market share is provided in the report.
-
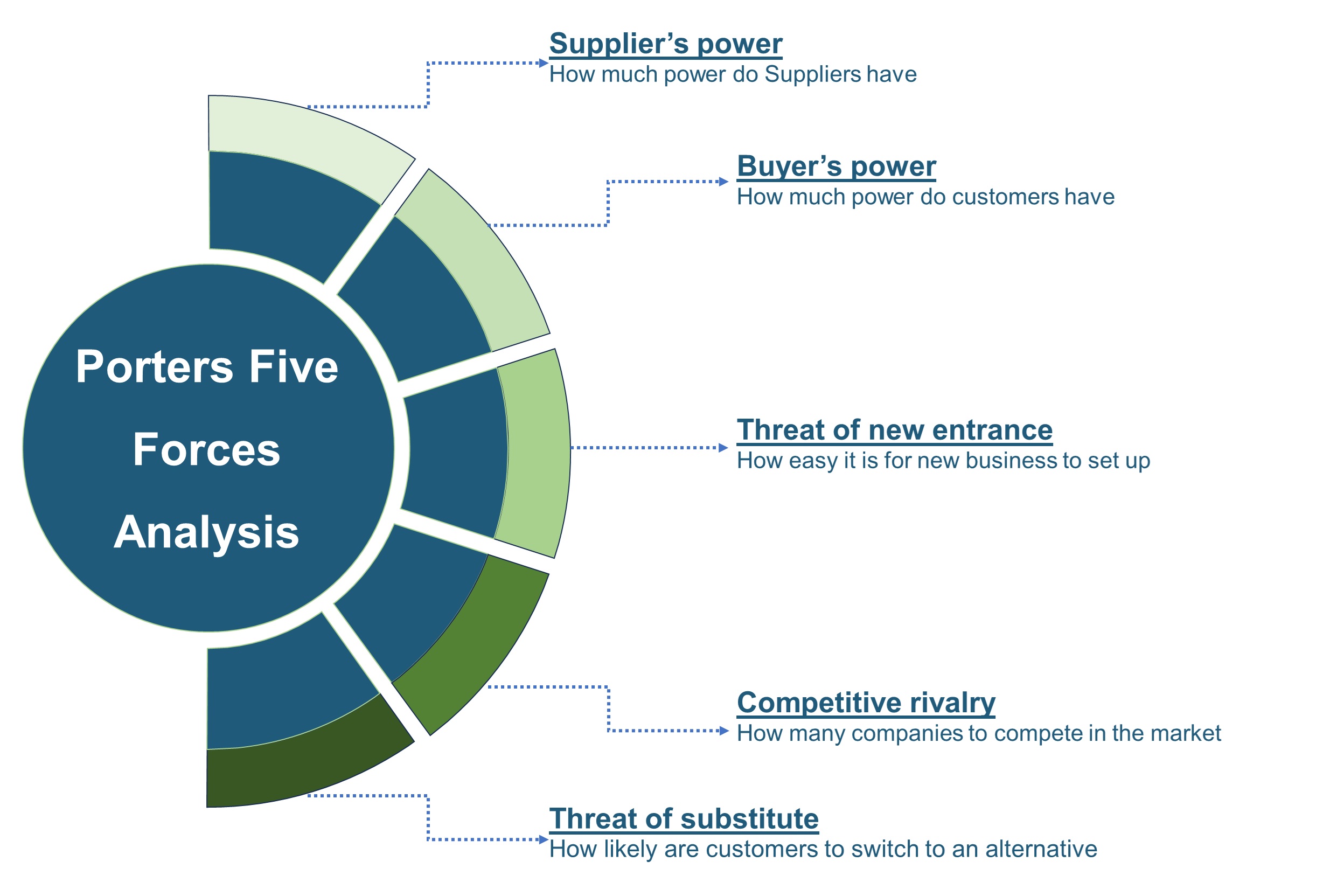
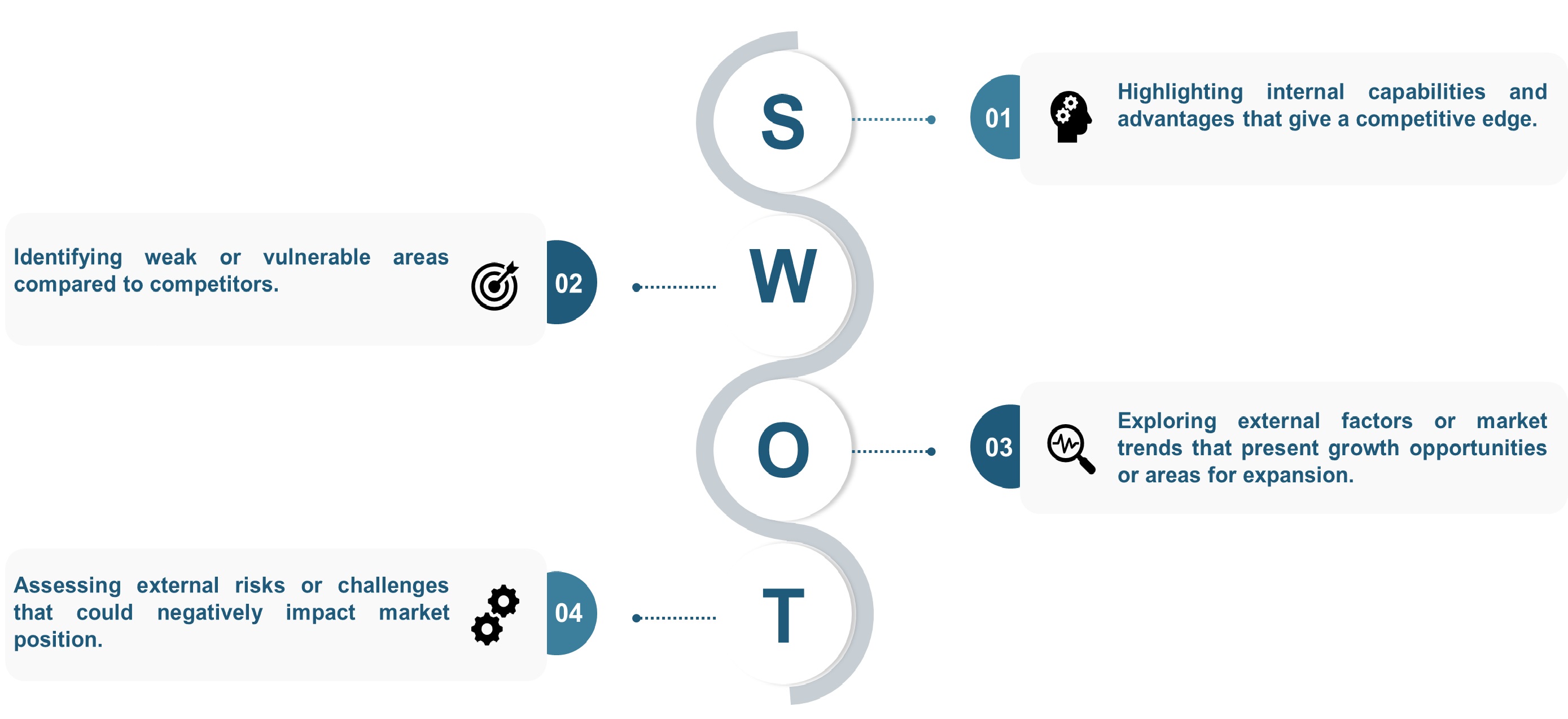
SWOT analysis and Porters Five Forces model is elaborated in the health insurance TPA market study.
-
Value chain analysis in the market study provides a clear picture of roles of stakeholders.
Health Insurance TPA Market Key Segments
By Insurance Type
-
Group Health Insurance
-
Individual Health Insurance
-
Others
By Service Type
-
Claims Processing
-
Pre-Authorization
-
Cashless Settlement
-
Customer Support
-
Hospital Network Management
By Deployment Model
-
In-House TPAs
-
Outsourced TPAs
By Sales Channel
-
Direct Selling
-
Agents
-
Brokers
By Enterprise Size
-
Small & Medium Enterprises (SMEs)
-
Large Enterprises
By End Users
-
Insurance Companies
-
Hospitals & Healthcare Providers
-
Corporate Sector
-
Others
By Region
-
North America
-
The U.S.
-
Canada
-
Mexico
-
-
Europe
-
The UK
-
Germany
-
France
-
Italy
-
Spain
-
Denmark
-
Netherlands
-
Finland
-
Sweden
-
Norway
-
Russia
-
Rest of Europe
-
-
Asia-Pacific
-
China
-
Japan
-
India
-
South Korea
-
Australia
-
Indonesia
-
Singapore
-
Taiwan
-
Thailand
-
Rest of Asia-Pacific
-
-
RoW
-
Latin America
-
Middle East
-
Africa
-
Key Players
-
United HealthCare Services, Inc (UMR)
-
WebTPA
-
Personify Health
-
Allied Benefit Systems, LLC
-
Meritain Health
-
Lucent Health
-
HealthEZ
-
PointC
-
Flores & Associates, LLC
-
Health Plans Inc
-
S&S Health
-
FirstEnroll
-
Luminare Health
-
ExpaTPA
-
Access Health Services
-
Euro Asistencia
-
AP Companies Group
-
WA Globality
Report Scope and Segmentation
|
Parameters |
Details |
|
Market Size in 2025 |
USD 235.29 Billion |
|
Revenue Forecast in 2030 |
USD 307.52 Billion |
|
Growth Rate |
CAGR of 5.50% from 2025 to 2030 |
|
Analysis Period |
2024–2030 |
|
Base Year Considered |
2024 |
|
Forecast Period |
2025–2030 |
|
Market Size Estimation |
Billion (USD) |
|
Growth Factors |
|
|
Countries Covered |
28 |
|
Companies Profiled |
15 |
|
Market Share |
Available for 10 companies |
|
Customization Scope |
Free customization (equivalent up to 80 working hours of analysts) after purchase. Addition or alteration to country, regional, and segment scope. |
|
Pricing and Purchase Options |
Avail customized purchase options to meet your exact research needs. |









 Speak to Our Analyst
Speak to Our Analyst